Since the time of the ancient Egyptians, alabaster, animal oils, salt, honey and sour milk were used for cutaneous aesthetic enhancements. Throughout the centuries thereafter, mankind has resorted to using various techniques to curb the advancement of ageor at least the appearance of old age. After countless iterations, one such technique has withstood astounding odds to become a popular method in the field of dermatology: chemical peeling.
Chemical peeling is defined as the chemical application of one or more chemical ablative agents to the skin’s surface to induce keratolysis or keratocoagulation. The subsequent destruction of all or part of the epidermis or dermis results in the exfoliation of these layers. Regeneration and remodeling of the epidermis or dermis improves the overall appearance and texture of the treated skin.
The earliest modern use of a chemical agent was back in 1871, when Tilbury Fox used 20% Phenol to lighten skin. Since then, numerous other techniques and agents have been used, such as trichloroacetic acid (TCA), salicylic acid (SA) and glycolic acid (GA). As our knowledge grows, the decision to use one particular agent over another has become dependent on the indication. This is due to variable penetration depth of chemical peeling agents.
Chemical peels are relatively straightforward for the treatment of pigmentary disorders, superficial acne scars, ageing skin changes, and benign epidermal growths. This technique has also been used to rejuvenate the skin of the face, neck, and hands.
Any medical professionals who are performing chemical peels must have adequate knowledge of the different peeling agents used, the process of wound healing, proper technique, and the identification and management of complications. Chemical peels may be used alone or in combination with other cosmetic procedures for cutaneous aesthetic enhancement.
Classification of chemical peels
There are a few ways to classify chemical peeling agents. They are divided into superficial, medium, and deep subtypes based on the depth of their penetration into the skin or based on their acid properties. Peeling agents that reach the papillary dermis but not the reticular dermis will be classified as superficial, while medium depth peels enter the superficial aspect of the reticular dermis. Lastly, deep peels extend all the way into the mid-reticular dermis. Keratolytics are primarily used for superficial and exfoliative procedures, whereas protein denaturants can be used for both superficial and/or deeper peels. Examples of keratolytic peeling agents are salicylic acid (1530%), glycolic acid (5070%), and phenol (2550%). Examples of protein denaturants are trichloroacetic acid (15100%), phenol (6088%), and the BakerGordon phenol peel (50% phenol, 2.1% croton oil).
Please note that the type of acid used, the concentration of the acid, rubbing force of the acid onto the skin, the volume of acid applied to the skin, whether or not the skin is preconditioned properly to enhance penetration, and in some peeling agents, the duration of contact of the acid on the skin all play an important role in determining the depth of penetration.
Protein denaturants will allow for deeper penetration than keratolytics. Additionally, higher concentration and volume solutions will penetrate deeper than lower concentrations and volumes. What’s more, the state of the patient’s skin can also affect the peel’s depth of penetration. For instance, thinner skin allows for deeper penetration; degreased skin absorbs acid faster, enhances peel penetration, and allows it to spread more evenly; and forceful application of the peeling agent will create deeper penetration.
Preparation for chemical peeling
Prior to treatment, consult the patient about any illnesses, medications, or conditions that may impair their wound healing or increase the risk of toxicity and infection (e.g. hepatic or renal disease, cardiac disease, diabetes mellitus, or immunosuppression). Note any other resurfacing procedures they’ve had done in the past, any history of herpes simplex infection, or abnormal scarring and photosensitivity, as these issues will increase the risk of complications. Dermatological conditions that may worsen with chemical peeling should also be noted. These include eczema, psoriasis, vitiligo, rosacea, and seborrhoeic dermatitis. The use of isotretinoin in the previous six to 12 months also increases the risk of delayed re-epithelialization and scarring. Additionally, the use of photosensitizing drugs, hormonal agents and oral contraceptives increases the risk of post-peel hyperpigmentation.
The pre-treatment regimen involves thinning the stratum corneum to enhance the penetration of the peeling agent and accelerate healing. These activities enhance patient compliance, detect intolerances, and reduce the risk of complications, such as post-inflammatory hyperpigmentation and scarring. They should be started at least two to four weeks before the chemical peel and stopped three to five days before. Tretinoin 0.0250.05% cream should be applied every night for a minimum of two weeks to begin thinning the stratum corneum. This will also increase epithelial differentiation and accelerate epithelial proliferation, hastening re-epithelialisation. In post-inflammatory hyperpigmentation-susceptible individuals, hydroquinone 2% to 4% should be started at least two weeks before a chemical peel. Other topical agents that may be used include glycolic acid, salicylic acid, kojic acid, azelaic acid, and topical corticosteroids.
Medium peels
Generally speaking, the deeper the site of pathology, the deeper the peel that will be required. Indications for medium depth peels are photoaging (e.g. static wrinkles, lentigines), superficial atrophic acne scars, and pigmentary disorders (e.g. post-inflammatory hyperpigmentation, freckles). They are usually performed with TCA in concentrations ranging from 20% to 35%, with a higher number of complications (i.e. scarring, hypopigmentation, hyperpigmentation) occurring at concentrations of 35% and above. Several combination treatments are now available that produce fewer side effects.
The vital ingredient in all above methods above is the TCA solution. As mentioned previously, it is a protein denaturant that acts as a medium-depth peeling agent. However, it is hydrophilic instead of lipophilic. As such, using keratolytics as the initial peeling agent helps to thin the skin and increase the permeability of the stratum corneum to allow better and more even penetration of the TCA solution.
Outcomes
The epidermis above the level of chemical injury will separate from the underlying skin on approximately the third day after treatment, and there will be some associated serous exudate and crusting. The skin tends to start to peel from the perioral area and radiate out to the whole face, with the forehead peeling last. Instruct them to not pick, rub, or scratch their skin during the healing process. After the epidermal peel layer has cleared, patients usually notice the new skin is brighter and more even. Pigmentation, blemishes and wrinkles should be reduced. After 6 weeks, neocollagenesis will occur, improving skin quality. Depending on the degree of photodamage and ageing, further peels may be needed to continue this rejuvenation.
After treatment, patients often complain of their skin feeling swollen and tight. Patients will also experience a moderate amount of facial edema within 48 hours. To help alleviate this issue, advise them to apply occlusive ointments and a moisturizer a few times per day. It is important during this time that patients avoid exercise and sun exposure. Every patient will have a different postoperative course, but, for the most part, patients should be fully healed within 78 days of the procedure. The patient’s pre-treatment skincare regime can be continued after 3 weeks.
Deep peels
Phenol has been mainly used as the peeling agent of choice for deep peels. TCA at 50% concentration has been reported to function as a deep peeling agent, but its complications are likely to outweigh its benefits.
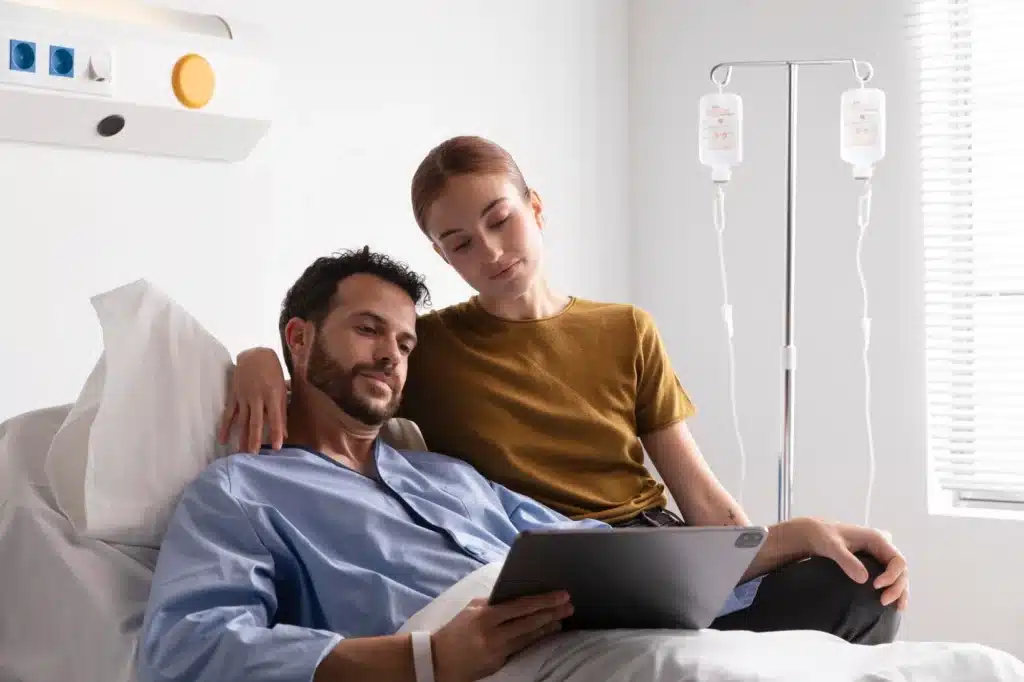
Performing similarly to TCA, phenol is a protein denaturant and coagulant. However, a crucial difference is that it penetrates the skin to the level of the reticular dermis faster. In addition, because phenol is systemically absorbed, toxicity resulting in cardiac arrhythmia has been observed. This is particularly important when treatment areas involve multiple sites. Therefore, it is essential that patients have their cardiac, renal, and hepatic function ascertained before attempting this technique. Cardiac monitoring and intravenous (IV) fluid hydration may also be necessary during the procedure.
A few formulations for phenol exist, though the years the Baker-Gordon formula developed in 1961 has remained popular. It consists of phenol, water, septisol soap, and croton oil, which allows for deeper penetration. Other formulas used olive oil and glycerin with phenol.
As the epidermolysis of a deep peel is complete, it will have far better improvements over severe wrinkles, dyschromia, and atrophic acne scars than lower-level peels. However, the risk of complication is much higher.
Outcomes
The downtime associated with deep phenol peels can be lengthy. To facilitate wound healing, occlusive dressings are needed after peeling. A waterproof tape mask is frequently used. Thymol iodide is also used several times a day for a week. The perioral area may undergo further damage and disruption of the wound healing process when it is allowed to move. Limit movements by introducing a blended diet via a straw. Epidermal re-epithelialisation should occur by approximately day nine. The new skin will be erythematous and swollen and, for very deep peels, can persist for up to four weeks. Phenol peels result in a dramatic and long-lasting improvement in facial rhytids, texture, and pigmentation.
Chemical peels complications
Generally, the deeper the peel, the more frequent and serious the complications. Most complications can be easily avoided by careful patient selection, using the appropriate peeling agent, introduction and adherence to a pretreatment regime, and close observation during all stages of treatment.
Prolonged erythema is an important manifestation of potential scarring. Although it is common immediately after peeling, it should fade within four weeks. Topical steroids, such as hydrocortisone, are an appropriate intervention technique given their pathophysiology. Other causes of erythema can be attributed to dermatological conditions, such as rosacea or eczema, contact sensitization, or unintentional peeling at a deeper depth.
Darker skinned individuals have an increased risk of developing more complications, such as permanent hypo-pigmentation, post-inflammatory hyperpigmentation, and scarring after medium and deep peels. Risks can be reduced with an adequate pre-treatment regime, but they are still unreasonably high in this patient group. For this reason, darker skinned patients should avoid deeper peels.
Identifying patients at risk should be the priority at the start of treatment. Risk factors such as darker skin type; sensitive skin or history of atopic dermatitis; dry skin and a reddish hue; outdoor occupations; history of photosensitivity or post inflammatory hyperpigmentation; taking photosensitizing drugs; history of keloids, poor wound healing or herpes infection; prior isotretinoin treatment; and unrealistic expectations should be determined before treatment with chemical peeling.
Summary
Any attempts at resurfacing the skin requires a considerable amount of pre-procedural planning to ensure reducing complications. Evaluate the patient to determine what is the correct procedure and depth of treatment required. For a successful peel procedure, all expectations for the procedure must be discussed with the patient and they need to understand well that they must readily participate in the post-peel care. Following the recommendations will ensure the best possible, longest-lasting results, especially when the results are followed up with use of products like Botox.