One of the most vexing problems dealt with in cosmetic surgery is acne scarring, an issue that affects 95% of patients with acne vulgaris and 111% of the general population. While this issue is widespread, a proper cure remains to be found: even with today’s technology, prevention remains the best remedy for acne scars.
This being said, a Cochrane Review published in 2016 found that injectable fillers may be the best solution on the current market. These products have been shown to treat atrophic acne scars, which are depressions in the skin.
Anatomy of acne scarring
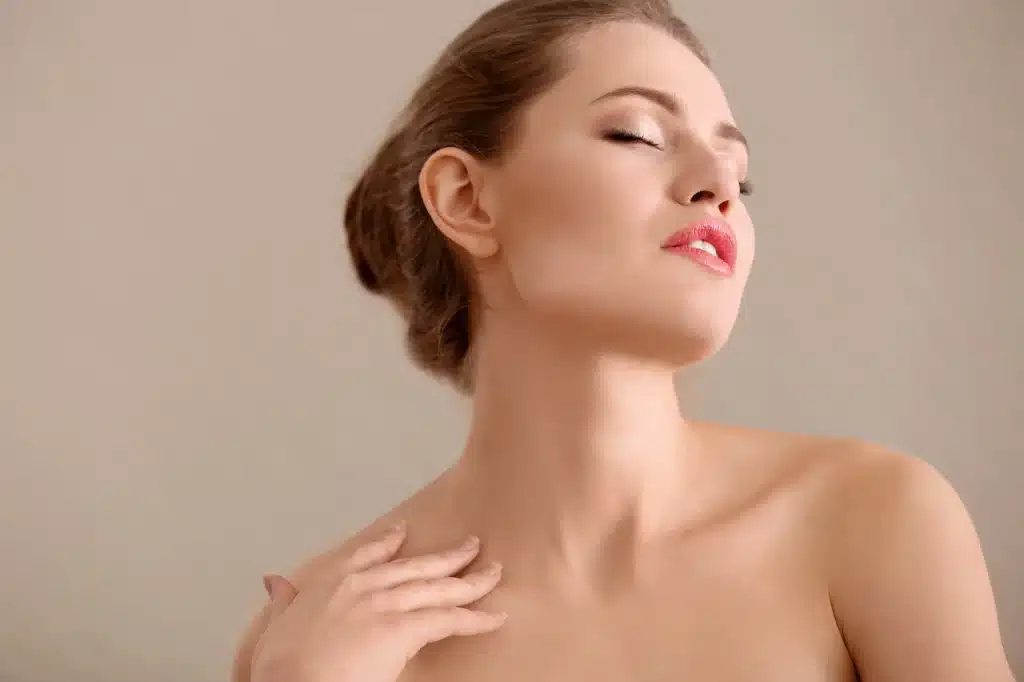
The steps involved in acne scar formation are complex. However, they generally involve an initial cutaneous inflammation, which is followed by an altered wound healing response, which causes an imbalance in matrix degradation and collagen biosynthesis. Overall, this leads to the formation of depressions in the skin, which are known as atrophic scars.
Current literature has identified three main forms of atrophic acne scars: ice pick scars, rolling scars and boxcar scars.
Ice pick scars Ice pick scars are V-shaped, narrow, and deep. They may extend into the deep dermis or subcutaneous tissue.
Rolling scars Rolling scars are wide and shallow. They produce an undulating appearance and are caused by the abnormal fibrous attachment of the dermis to the subcutis.
Boxcar scars Boxcar scars are widest at the base. These round- to oval-shaped skin dimples have sharp margins and can be either shallow or deep.
How do hyaluronic acid fillers heal scars?
Today, medical professionals use hyaluronic acid fillers to smooth uneven skin texture caused by acne scarring. When injected into the tissue underneath scars, these products plump up indentations and fill them out with their volumizing power. These temporary products are widely used in the US, and are known to have an excellent safety profile, high efficacy, and an easy-to-follow injection process.
Pros and Cons of Hyaluronic Acid
Pros:
- Lasts 612 months, although duration may vary from patient to patient
- Temporary treatment that can be reversed if outcome is unsatisfactory
- Hyaluronic acid is a naturally-derived substance that is generally well-tolerated by most patients
- Many formulas come pre-mixed with lidocaine for effective pain relief
Cons:
- Injection-related side effects, including bleeding, swelling, and pain at the injection site, are common; however, these usually subside within 1-week post-injection
- Requires follow-up treatments
Is Hyaluronic Acid effective for acne scarring?
The efficacy of hyaluronic acid in treating acne scars is supported by a few studies. However, the current modalities for acne scar treatment aim only to make scars less visiblethey cannot cure them entirely. This rings true with hyaluronic acid fillers as well. Keep in mind that some scars may respond better to treatment than others, as the type and depth of scar tissue plays a considerable role in determining its efficacy. Rolling and boxcar scars are said to have the best response to hyaluronic acid injections.
Many patients will most likely have spent a significant portion of their lives seeking to rid themselves of their acne scars. As such, many are still appreciative of even slight improvements to their appearance. With this, hyaluronic acid fillers are a wonderful option for susceptible patients.
What are dermal fillers?
A dermal filler is classified by the Food and Drug Administration (FDA) as a medical device that
is placed into the dermis to create a smoother and fuller appearance in the skin. Besides hyaluronic acid, dermal fillers can be made from a variety of biomaterials, such as silicone, polyacrylamide, calcium hydroxylapatite, and poly-L-lactic acid. As mentioned earlier, the duration of action of fillers is variable, which is mainly due to their biodegradability.
Hyaluronic acid (HA)
Multiple HA fillers have been approved by the FDA. They differ based on their rheological properties, and therefore cannot be used interchangeably. FDA approved HA fillers include Juvederm (Allergan), Restylane and Perlane (Galderma), Prevelle (Mentor), and Belotero (Esthelis Merz). Though the primary use for HA has been for static rhytids and for volumization (i.e. lip/cheek augmentation), their use in acne scars has seen tremendous development. Though the sample size for the studies mentioned above are small, almost all showed improvements in acne scar appearance with minimal adverse effects.
Poly-L-lactic acid (Sculptra)
Poly-L-lactic acid (PLLA) is a semi-permanent form of filler that lasts up to 2 years. It was used initially to correct facial lipoatrophy caused by human immunodeficiency virus (HIV). Four studies have shown the efficacy of PLLA on acne scars so far, and all showed positive outcomes. The sample size ranged from 1 to 22 patients, and very minimal adverse effects and significant reductions in acne scar size and severity were witnessed.
Polymethylmethacrylate (Bellafill)
Polymethylmethacrylate (PMMA) is a permanent filler, which means it is capable of lasting longer than 3 years. It has retained FDA approval for use in acne scarring since 2015. 3 studies were conducted which demonstrated the benefit of PMMA in atrophic acne scars. The largest double-blind, randomized, controlled trial (RCT) to date (n = 147) used 2 treatment sessions with a 6-month follow-up, and demonstrated that PMMA provided a statistically significant superior treatment for atrophic facial acne scarring of 64%, versus 33% in the control arm (P = 0.0005). A single-center, open-label, pilot study of 14 patients with atrophic acne scars that underwent subcision prior to PMMA injection found that 96% of them experienced scar improvement at 8 months post-treatment, with no adverse effects reported. This being said, complications with PMMA can occur, and usually include tissue necrosis, chronic inflammatory reactions, lymphedema, and infections.
Complications
Early side effects
Because the injection techniques for dermal fillers may involve multiple jabs to the treatment area, transient post injection bruising, swelling, and erythema is common and expected. However, these issues will self-resolve within a few days to weeks. Prolonged swelling can be treated with ice compression and oral antihistamines.
For the subject of side effects, it is imperative that trained medical professionals perform these procedures, as an improper injection may cause multiple serious side-effects. If injected incorrectly, tissue ischemia may be one of the issues to occur. This will appear in the form of blanching in certain areas, or alternatively as a violaceous reticular pattern. If unwanted issues like this occur, attempt to revascularize the area immediately, thoroughly massaging the area, applying heat packs, and injecting 10 to 30 units of hyaluronidase within the treatment site. Also ensure the patient is provided 2 tablets of aspirin. To minimize the occurrences of these events, ensure that you, as a specialist, are proficient in injection techniques specific to this product prior to practicing on a patient.13
Delayed side effects
After injection, inflammatory nodules may occur. These should be treated as bacterial infections. Furthermore, granulomas may appear 6 to 12 months post-injection. To treat these, use intralesional steroid injection or excision.
Technique
The technique used will determine the outcome of the procedure, as well as possible complications. As such, proper training is imperative. It is also important to work in a methodical manner, so that no scar tissue is missed.
Lifting out individual scars:
- Position the patient in a semi-reclined position at about 65 degrees with their head rested on a pillow. Prepare the skin with alcohol and take a pre-injection photograph. This will be used to scrutinize the results after the injection.
- Anesthetize the area using the least amount of local anesthetic possible to reduce pain during injection.
- Prime the needle by depressing the syringe plunger until a droplet of the dermal filler is visible at the tip. Please ensure that the needle is firmly attached to the syringe to prevent the syringe from disconnecting.
- Advance the needle into the skin. You will know that your needle is in the dermis when you feel a slight resistance and the needle tip is no longer visible in the skin.
- Inject with a firm and constant pressure, continuing to place product into the skin as you withdraw the needle. Stop putting pressure on the plunger when you are near the surface of the skin.
- Repeat as needed until you are satisfied with the results.
- Refer to the pre-procedure photograph to ensure that all required scars have been injected.
- Massage the skin after each injection. Working systematically is important, because local edema will result in difficulty recognizing the scars. When edema has developed to this point, stop the current procedure and proceed during the next treatment cycle.13
Conclusion
The demand for treatment for acne scars will always remain high due to the prevalence of acne vulgaris. Over the course of your practice, you will inevitably be asked to provide evaluation and treatment recommendations. You may be overwhelmed by all the choicesmedical, surgical, and procedural optionssince they are all historically proven to lessen the severity of acne scars, but you will find that most are cumbersome and expensive. The good news is that the treatment of acne scarring is evolving in a way that is beneficial to both the patient and the practitioner. The idea of tissue augmentation and volume replacement and our understanding of what can be achieved with these methods is increasing rapidly as more studies are being conducted. Because of this, we are seeing safer and longer lasting biomaterials in the correction of significant atrophic acne scarring.
Dermal fillers are an excellent option for minimally invasive rejuvenation. They provide tangible results in a reasonable amount of time and have close to no downtime for the patient. The complications can be predicted and prevented as long as you select the appropriate filler and use the correct technique of injection. Outcome can be further optimized when you also understand the differences between fillers, evaluate the defect accurately, and most importantly, discuss realistic expectations with your patients. Remember: improvement in the appearance of acne scarring, rather than complete elimination, is the goal.