According to the Centers for Disease Control and Prevention (CDC), the human papillomavirus (HPV) vaccine significantly lowers the risk of developing HPV-related cancers. The vaccine is most effective when administered during adolescence, making early vaccination crucial for long-term protection.
Gardasil, a leading HPV vaccine, is recommended for individuals starting as young as 9 years old. It protects against multiple high-risk HPV strains linked to cancers and genital warts, highlighting the importance of understanding the ideal timing for vaccination to ensure maximum effectiveness.
In this article, we’ll explore the recommended ages for Gardasil vaccination and discuss why the timing of the vaccine is vital to optimal protection.
Key Takeaways
- Gardasil vaccination protects against human papillomavirus (HPV) and related diseases.
- The ideal age for receiving the Gardasil vaccine is between 9 and 14 years old before potential exposure to HPV.
- Catch-up vaccination is available for older adolescents and adults up to age 45.
- Clinical guidelines and expert recommendations support the importance of timely Gardasil vaccination for optimal protection.
About: Medical Spa RX provides medical practices with premium products at the best prices. If you’re looking to order Gardasil online for your practice, the sales representatives at Medical Spa RX can give you guidance.
The Importance of Gardasil Vaccination

Gardasil is a crucial vaccine designed to protect against certain strains of human papillomavirus (HPV). HPV is a common sexually transmitted infection that can lead to various health issues, including genital warts and certain cancers. The vaccine primarily targets the most high-risk HPV types associated with cervical, anal, and oropharyngeal cancers.
Benefits of Gardasil
- Cancer Prevention: Gardasil provides robust protection against HPV-related cancers. By vaccinating individuals before they become sexually active, we can significantly reduce the risk of developing cervical, anal, and other HPV-associated cancers.
- Genital Wart Prevention: In addition to cancer prevention, Gardasil also helps prevent genital warts caused by HPV. These warts can be uncomfortable, unsightly, and emotionally distressing.
- Herd Immunity: Widespread vaccination contributes to herd immunity, protecting even those who haven’t received the vaccine. When a significant portion of the population is vaccinated, the overall transmission of HPV decreases, benefiting everyone.
Early vaccination is essential. Ideally, individuals should receive the Gardasil vaccine before they become sexually active. The vaccine is most effective when administered before exposure to HPV. However, even if someone has already been exposed to one or more strains, Gardasil can still protect against the remaining strains.
They may also speak with a qualified healthcare provider to learn more about Gardasil and HPV and other strategies to avoid this type of viral infection.
Recommended Age Range for Gardasil Vaccination

The ideal time to receive the Gardasil vaccine is between the ages of 9 and 14. Here’s why:
- Early Protection: Vaccinating individuals before they become sexually active ensures early protection against HPV. The vaccine is most effective when administered before exposure to the virus.
- Robust Immune Response: Younger recipients tend to mount a stronger immune response to the vaccine. This enhances their ability to fight off HPV infections.
- Complete Series: Gardasil is administered in a series of doses. Starting early allows individuals to complete the full vaccination schedule before potential exposure.
Early vaccination is crucial because it offers the best chance of preventing HPV infections before any risk of exposure. Starting the series at ages 11 or 12—and even as early as age 9—ensures that the vaccine can work proactively, providing long-term protection against the most harmful strains of HPV.
It contributes to individual health and also plays a significant role in public health by reducing the overall prevalence of HPV-related diseases, including cervical and throat cancers.
Catch-Up Vaccination for Older Adolescents and Adults

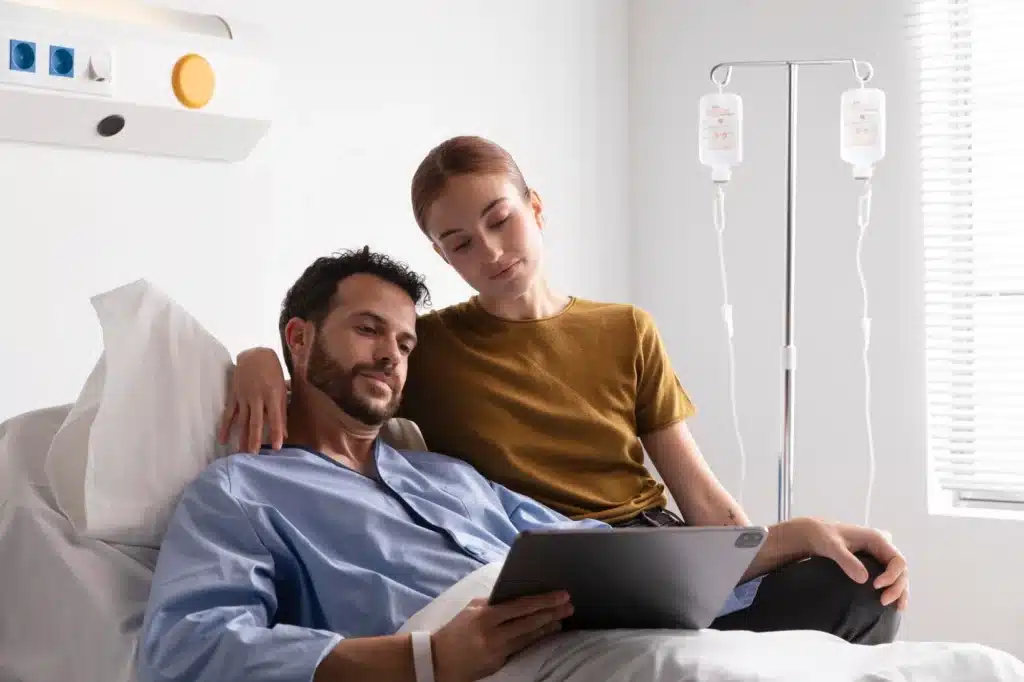
Catch-up vaccination is available for older adolescents and adults who did not receive Gardasil at the recommended age. This option allows individuals up to the age of 45 to benefit from the vaccine’s protective effects against HPV-related cancers and genital warts, even if they missed earlier vaccination opportunities.
The recommended age limit for catch-up vaccination is up to 26 years, but it is also offered to individuals aged 27 to 45 based on individual risk factors and healthcare provider recommendations. Although the vaccine is most effective when administered at a younger age, it can still provide significant benefits for those who may have already been exposed to HPV.
Importance of Vaccination for Older Individuals
- Reducing Risks: Catch-up vaccination helps reduce the risk of HPV-related cancers and genital warts, even if an individual has already been exposed to some HPV strains.
- Individual and Community Health: By vaccinating older adolescents and adults, we contribute to herd immunity and protect vaccinated individuals and those around them.
Clinical Guidelines and Expert Recommendations
Clinical guidelines from the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) recommend starting Gardasil vaccination at age 9, with the ideal vaccination age being 11 to 12. For those who miss this preferred window, catch-up vaccinations are recommended up to age 26, and in some cases, up to age 45, depending on individual circumstances and risk factors.
Experts stress the importance of vaccinating before exposure to HPV, which often occurs shortly after the onset of sexual activity. Administering the vaccine during the preteen years helps ensure a strong immune response, providing long-lasting protection against the most dangerous HPV strains.
Healthcare professionals advocate for early vaccination as it maximizes the vaccine’s effectiveness and plays a crucial role in reducing the incidence of HPV-related cancers. Even for those vaccinated later in life, Gardasil offers valuable protection against HPV strains they may not have been exposed to yet, underscoring its importance at any age.
Conclusion
Vaccination with Gardasil at the recommended age is crucial for effective protection against HPV-related diseases. Starting as early as age nine can significantly reduce the risk of developing these conditions later in life.
However, Gardasil is not a substitute for regular cancer screenings and may not provide complete protection for everyone. To ensure comprehensive health protection, it’s essential to follow your healthcare provider’s guidance on vaccination timing and continue routine screenings.
FAQs
1. What is Gardasil?
Gardasil is a vaccine that protects against certain types of human papillomavirus (HPV). HPV can cause cancers and other health issues, so getting vaccinated helps prevent these problems.
2. When should I get vaccinated with Gardasil?
The best time to get the Gardasil vaccine is between ages 11 and 12. However, it’s also safe for teens and young adults up to age 26. If you missed this window, talk to your doctor about getting it later.
3. How many doses of Gardasil do I need?
Most people need two or three doses of the Gardasil vaccine, depending on their age when they start the series. For maximum protection, it’s important to follow the schedule your healthcare provider gives you.
4. Are there any side effects from the Gardasil vaccine?
Like all vaccines, Gardasil can have side effects. Most are mild, like soreness at the injection site or fever. Serious side effects are rare but possible; always discuss concerns with your doctor before vaccination.
References
Centers for Disease Control and Prevention. (2021). Human papillomavirus (HPV) vaccination: What everyone should know. https://www.cdc.gov/vaccines/vpd/hpv/public/index.html
Ellingson, M. K., Sheikha, H., Nyhan, K., Oliveira, C. R., & Niccolai, L. M. (2023). Human papillomavirus vaccine effectiveness by age at vaccination: A systematic review. Human vaccines & immunotherapeutics, 19(2), 2239085. https://doi.org/10.1080/21645515.2023.2239085
Lake, P., Fuzzell, L., Brownstein, N. C., Fontenot, H. B., Michel, A., McIntyre, M., Whitmer, A., Rossi, S. L., Perkins, R. B., & Vadaparampil, S. T. (2023). HPV vaccine recommendations by age: A survey of providers in federally qualified health centers. Human vaccines & immunotherapeutics, 19(1), 2181610. https://doi.org/10.1080/21645515.2023.2181610